Conclusion of the Clinical Research Framework Proposal for Ketogenic Metabolic Therapy in Glioblastoma
Introduction
This article serves as a conclusion to the original clinical research framework proposal for ketogenic metabolic therapy (KMT) in glioblastoma (GBM) treatment. As one of the most aggressive forms of cancer, GBM presents significant challenges in terms of effective treatment and patient prognosis. The original proposal outlines a structured approach to exploring KMT as a complementary strategy to traditional therapies. Here, we summarize the key insights and implications of this innovative treatment approach. For the full details, please refer to the original source: Clinical research framework proposal for ketogenic metabolic therapy in glioblastoma by Tomás Duraj et al., published in BMC Medicine, Volume 22, Article number: 578 (2024).
Understanding Glioblastoma and Its Metabolic Characteristics
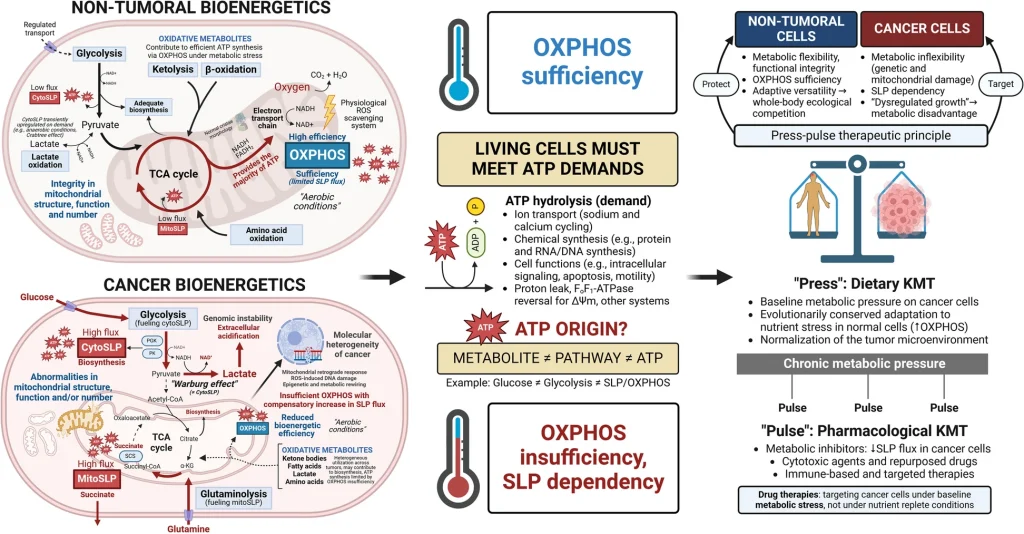
GBM cells exhibit unique metabolic characteristics that distinguish them from normal brain cells. They primarily rely on glucose and glutamine for energy and growth, utilizing glycolysis and glutaminolysis to meet their anabolic demands. This metabolic dependency presents a therapeutic opportunity: by targeting these pathways, it may be possible to inhibit tumor growth and improve patient outcomes.
What is Ketogenic Metabolic Therapy (KMT)?
KMT is a dietary intervention that shifts the body’s metabolism from glucose to ketones, which are produced from fat. This metabolic shift can create a hostile environment for cancer cells, which are less efficient at utilizing ketones compared to glucose. KMT involves a high-fat, low-carbohydrate diet, often combined with calorie restriction and fasting, to induce a state of therapeutic ketosis. The goal is to reduce the availability of glucose and glutamine, thereby starving GBM cells of their primary energy sources.
Overview of Potential Drug Treatments as Part of KMT Research
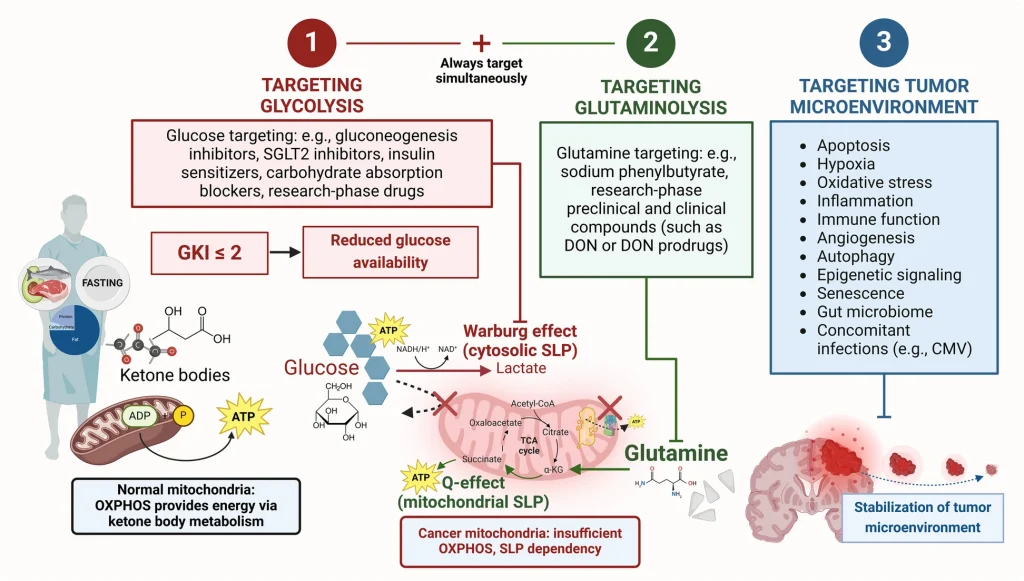
As part of the KMT research framework, potential drug treatments can be categorized into three strategic areas: glucose targeting (red), glutamine targeting (green), and tumor microenvironment stabilization (blue).
- Glucose Targeting (Red): Safe administration of metabolic inhibitors will require physiological adaptation to a GKI-adjusted ketogenic diet (KD) or ketogenic diet with restriction (KD-R), which can be accelerated by water-only fasting. Once this adaptation is achieved, glycolysis targeting can be considered to further improve the glucose-ketone index (GKI) and slow tumor progression. Potential agents include antidiabetic medications such as metformin or SGLT2 inhibitors, as well as research-phase glycolytic inhibitors.
- Glutamine Targeting (Green): Concurrently, glutaminolysis should be targeted using agents such as sodium phenylbutyrate, 6-diazo-5-oxo-L-norleucine (DON), or novel glutamine inhibitors. This dual approach aims to effectively starve GBM cells of both primary energy sources.
- Tumor Microenvironment Stabilization (Blue): Finally, normalization of the tumor microenvironment can be explored in a modular fashion. Strategies may include targeting cell proliferation with mebendazole, reducing inflammation with non-steroidal anti-inflammatory drugs (NSAIDs), addressing hypoxia through hyperbaric oxygen therapy (HBOT), restoring redox balance with dichloroacetate (DCA) or intravenous vitamin C, and exploring immunotherapy or combinatory approaches such as CUSP9.
Linking to the Clinical Research Framework Proposal
The original clinical research framework proposal for KMT in glioblastoma outlines a structured approach to investigating the efficacy of this therapy. Key components of the proposal include:
- Study Design: The framework emphasizes the importance of randomized controlled trials (RCTs) to provide robust evidence for KMT’s effectiveness in GBM treatment.
- Patient Selection: It highlights the need for careful patient selection based on tumor characteristics and metabolic profiles, ensuring that the most appropriate candidates are chosen for KMT.
- Intervention Protocol: The proposal details a comprehensive intervention protocol that includes a GKI-adjusted ketogenic diet, metabolic inhibitors, and real-time monitoring of compliance through the glucose-ketone index (GKI).
- Outcome Measures: The framework outlines primary and secondary outcome measures, focusing on survival rates, quality of life, and metabolic markers.
- Ethical Considerations: Ethical implications are addressed, emphasizing the importance of informed consent and patient education in the context of novel therapies.
The Promise of KMT in GBM Treatment
Emerging evidence suggests that KMT may enhance the effectiveness of conventional therapies by targeting the metabolic vulnerabilities of GBM cells. By depriving these cells of their preferred energy sources, KMT has the potential to slow tumor growth and improve patient survival. Additionally, the integration of KMT with existing treatment modalities could lead to synergistic effects, offering a more comprehensive approach to GBM management.
Conclusion
As the fight against glioblastoma continues, innovative strategies like ketogenic metabolic therapy offer hope for improved patient outcomes. The clinical research framework proposal serves as a vital roadmap for future studies, guiding researchers in the exploration of KMT’s potential in GBM treatment. By understanding and targeting the unique metabolic characteristics of GBM cells, we may pave the way for more effective and personalized therapies in the battle against this formidable cancer.
Call to Action
For those interested in the intersection of nutrition and cancer therapy, the exploration of ketogenic metabolic therapy in glioblastoma represents an exciting frontier. Researchers, clinicians, and patients alike are encouraged to engage with ongoing studies and contribute to the growing body of evidence supporting this innovative approach. Together, we can advance the understanding of KMT and its role in transforming glioblastoma treatment.
